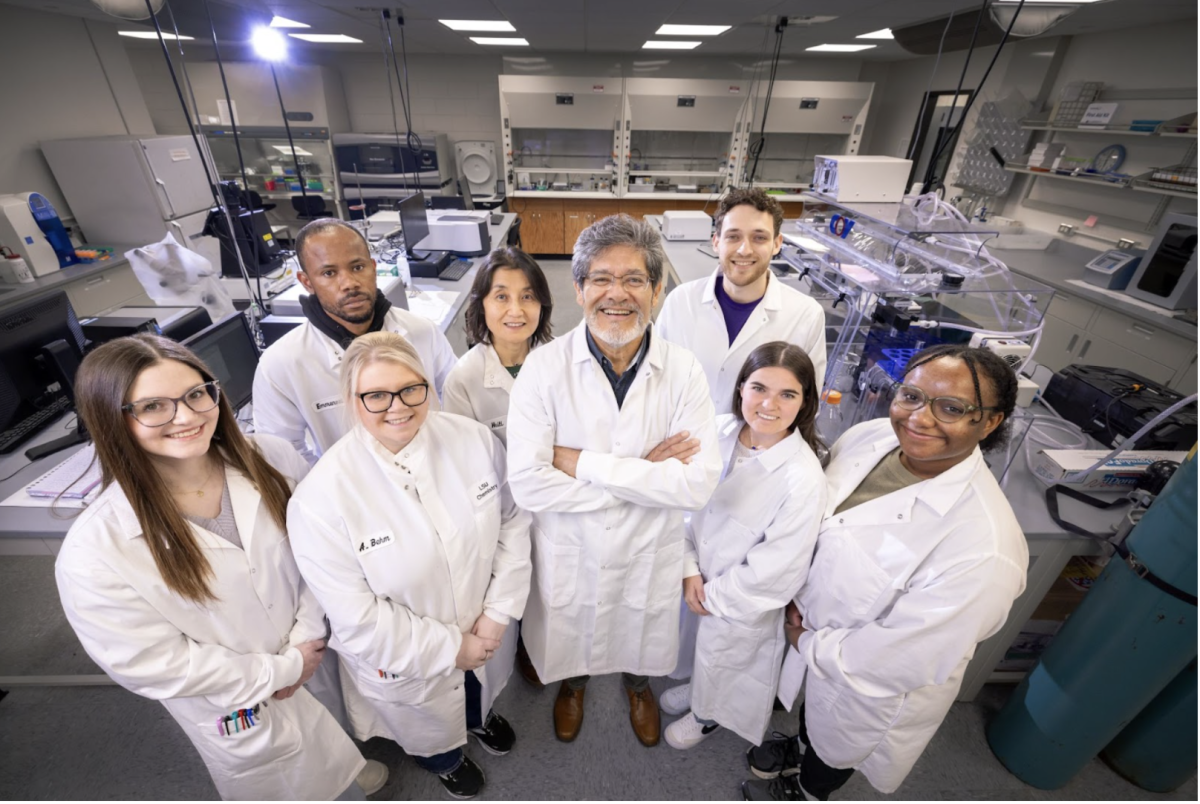
Physics professor Guang Jia and medical physics doctoral candidate Joseph Steiner are revolutionizing prostate cancer screening by developing a device to increase accuracy.
If successful, their device will produce more accurate CT scans of the prostate and improve prostate cancer diagnoses.
Current screening methods, including the prostate-specific antigen test and the digital rectal exam, have a wider margin of error than Jia and Steiner’s proposed technique. PSAs can be released for a variety of prostate diseases, not only cancer, and DREs may not detect small or obscurely located tumors, Jia said.
The device involves attaching an intraoral sensor to an inner rectal coil to produce higher image resolution when used in conjunction with a CT scan. The intraoral sensor is used in dental radiography and inner rectal coils are traditionally used in MRIs, Jia said.
“That’s the good thing about what we’re trying to do,” Steiner said. “Everything’s already been done, and we’re just mashing everything together.”
Traditional prostate CT scans use a surface coil, which has difficulty producing a detailed image of the prostate because of the organ’s small size and central location. An internal sensor will localize the CT radiation and produce a clearer image of the prostate, Jia said.
“This is like during the day, if there’s a street lamp you might not identify it from the bright sky,” Jia said. “But if you put your eyes very close to the lamp, you cannot ignore it. The detector is our eye, and the prostate is the lamp.”
The digital detector has 100 times smaller pixels than a CT scan, producing scans with 10 times higher resolution, Jia said.
The device is being tested using an imaging phantom — an
object used in scanners to evaluate imaging devices — and a kumquat at Mary Bird Perkins Cancer Center, Steiner said. The kumquat is similar in size and shape to a human prostate and provides greater imaging potential because it is made of biological tissue.
After perfecting their technique on the kumquat, tests will begin on canine prostates donated by the LSU School of Veterinary Medicine. A 3-D printer will be used to produce a model of either the canine or human lower body to test the detector using more naturalized dimensions, Jia said.
It will likely be two years before testing is complete and the device moves on to human trials, Steiner said.
“Because this has never been done before it’s kind of exploratory research,” he said. “You have to start at the bottom and work your way up.”
Exploration includes optimizing the CT scanner to produce the best image for the lowest dose of radiation, Jia said. This requires testing radiation levels, exposure, tilt angles and additional factors to produce the most efficient results.
Outside of screening, Jia and Steiner’s method can be used to target cancer treatments such as brachytherapy treatment, which uses radioactive seeds to provide low-dose radiation to a small area of the body. Detailed screening will allow doctors to target the brachytherapy seeds’ injection to ensure correct placement and improved treatment, Steiner said.
The device may also be used to screen higher risk cancers including cervical cancer and rectal cancer, Steiner said. Though more expensive and uncomfortable for the patient than a PSA or DRE, Jia and Steiner’s technique could reduce the number of procedures a patient undergoes and minimize associated medical risks.
“If the benefits outweigh the costs, it’ll be a viable solution,” Steiner said.
Jia and Steiner submitted a patent application for their device through the LSU Office of Innovation and Technology Commercialization on July 29.
Professor, doctoral candidate develop device to improve prostate cancer screening
February 2, 2016
LSU associate professor Kip Matthews, associate professor Dr. Guang Jia, and graduate student Joe Steiner displaying their x-ray technique and equipment for the detection and curing of prostate cancer on Monday Jan. 25, 2016, in Nicholson Hall on LSU campus.
More to Discover